COVID-19 Drops Off U.S. Top 10 Causes of Death List in 2024: A Turning Point?
For the first time since 2020, COVID-19 is no longer among the top 10 leading causes of death in the United States. This significant shift, observed in early 2024 data, signals a potential turning point in the nation’s battle against the virus. While COVID-19 remains a concern, its reduced impact on mortality rates reflects the combined effects of vaccination, improved treatments, and potentially, evolving viral strains. This article delves into the implications of this change, exploring the factors contributing to the decline and what it means for the future of public health.
Understanding the Shift: COVID-19 Mortality Trends
The COVID-19 pandemic dramatically altered mortality landscapes globally. In 2020, it surged to become the third leading cause of death in the U.S., behind only heart disease and cancer. Throughout 2021 and 2022, COVID-19 remained a prominent cause of death, claiming countless lives and straining healthcare systems. However, recent data indicates a substantial decrease in COVID-19-related deaths, pushing it outside the top 10.
Several factors have contributed to this positive trend:
- Widespread Vaccination: Vaccination campaigns have significantly reduced the severity of COVID-19 infections and, consequently, the risk of hospitalization and death. Booster doses have further enhanced protection, particularly among vulnerable populations.
- Improved Treatments: The development and availability of antiviral medications like Paxlovid and monoclonal antibody treatments have played a crucial role in reducing the severity of illness and preventing fatal outcomes.
- Evolving Viral Strains: While new variants continue to emerge, many have exhibited reduced virulence compared to earlier strains like Delta. This has led to milder infections and lower mortality rates.
- Increased Immunity: A combination of vaccination and prior infection has likely contributed to a higher level of population immunity, reducing the overall risk of severe illness.
- Enhanced Public Health Measures: While many restrictions have been lifted, ongoing public health recommendations, such as staying home when sick and practicing good hygiene, continue to play a role in mitigating transmission.
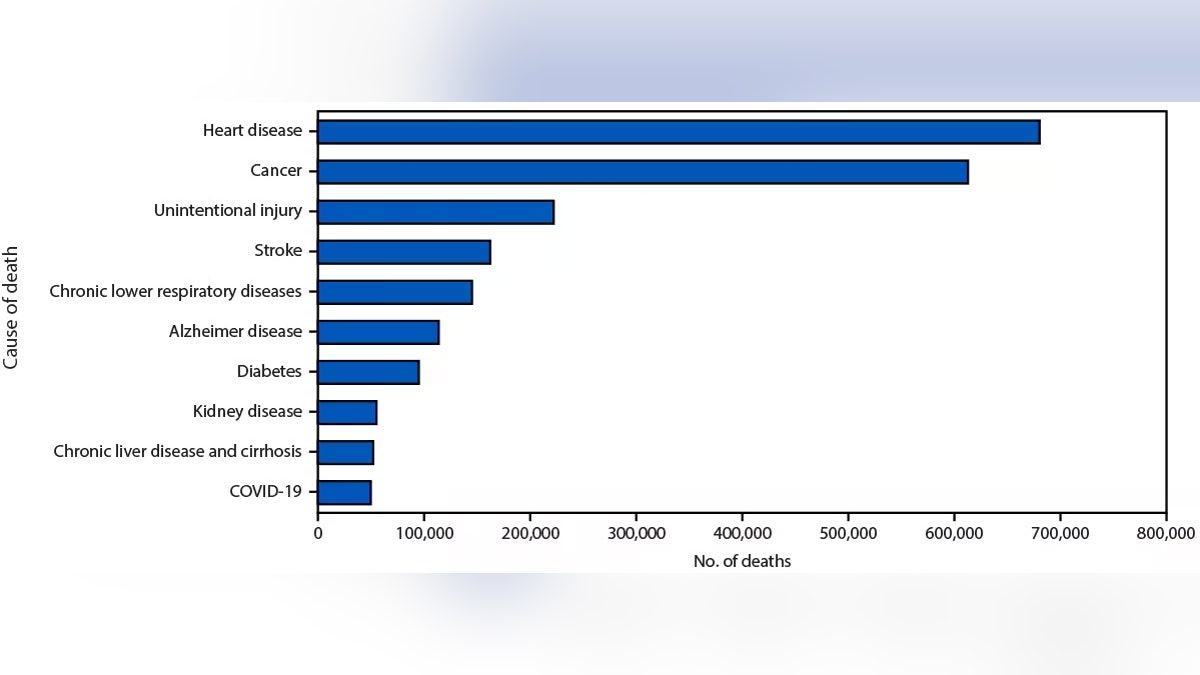
What Replaces COVID-19 in the Top 10?
With COVID-19’s exit from the top 10, other causes of death that were previously overshadowed have regained prominence. These often include chronic diseases, accidents, and other infectious diseases. The specific order of the top 10 causes can fluctuate based on data collection periods and variations in reporting, but generally include:
- Heart Disease
- Cancer
- Accidents (Unintentional Injuries)
- Stroke (Cerebrovascular Diseases)
- Chronic Lower Respiratory Diseases
- Alzheimer’s Disease
- Diabetes
- Influenza and Pneumonia
- Kidney Disease
- Suicide
Implications for Public Health and Future Preparedness
The decline of COVID-19 as a leading cause of death is undoubtedly a positive development. It allows healthcare systems to allocate resources more effectively and potentially address other pressing public health concerns. However, it’s crucial to remain vigilant and maintain preparedness for future outbreaks.
- Continued Monitoring: Ongoing surveillance of COVID-19 and other respiratory viruses is essential to detect emerging variants and track transmission patterns.
- Vaccination Efforts: Sustained efforts to promote vaccination and booster uptake, particularly among vulnerable populations, are crucial for maintaining protection.
- Investment in Research: Continued investment in research to develop new vaccines, treatments, and diagnostic tools is vital for future pandemic preparedness.
- Strengthening Public Health Infrastructure: Strengthening public health infrastructure, including disease surveillance systems and healthcare capacity, is essential for responding effectively to future health emergencies.
- Addressing Health Disparities: COVID-19 has disproportionately impacted certain communities. Addressing underlying health disparities is crucial for ensuring equitable access to healthcare and preventing future crises.
The Path Forward: Living with COVID-19
While COVID-19 may no longer be a top killer, it’s important to recognize that it hasn’t disappeared entirely. It’s likely to become an endemic disease, circulating at lower levels and causing seasonal outbreaks. Learning to live with COVID-19 involves:
- Staying Informed: Keep abreast of the latest public health recommendations and guidelines.
- Practicing Preventative Measures: Continue to practice good hygiene, such as handwashing and covering coughs and sneezes.
- Seeking Medical Care: Consult a healthcare provider if you experience symptoms of COVID-19.
- Staying Up-to-Date on Vaccinations: Ensure you are up-to-date on your COVID-19 vaccinations and boosters.
Conclusion
The removal of COVID-19 from the top 10 causes of death in the U.S. is a significant milestone in the ongoing fight against the virus. It reflects the success of vaccination efforts, improved treatments, and evolving viral strains. While vigilance and preparedness remain crucial, this shift offers a glimmer of hope and a chance to refocus on other pressing public health challenges. By continuing to learn and adapt, we can build a more resilient and healthier future.
Frequently Asked Questions (FAQs)
Q1: Does this mean COVID-19 is no longer a threat?
No. While COVID-19’s impact on mortality has decreased significantly, it still poses a risk, especially to vulnerable populations. It’s likely to become an endemic disease, meaning it will continue to circulate at lower levels.
Q2: Should I still get vaccinated against COVID-19?
Yes. Vaccination remains the most effective way to protect yourself and others from severe illness, hospitalization, and death from COVID-19. Staying up-to-date on boosters is also recommended.
Q3: What are the long-term effects of COVID-19?
Some individuals experience long-term health problems after a COVID-19 infection, known as “long COVID.” These can include fatigue, shortness of breath, cognitive difficulties, and other symptoms. Research is ongoing to better understand and treat long COVID.
Q4: How can I protect myself from COVID-19 now that restrictions have been lifted?
Continue to practice good hygiene, such as handwashing and covering coughs and sneezes. If you are feeling unwell, stay home to avoid spreading the virus. Consider wearing a mask in crowded indoor settings, especially if you are at higher risk of severe illness.
Q5: Where can I find the most up-to-date information on COVID-19?
Reliable sources of information include the Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/) and your local health department.